Symptoms of Digital Mucous Cyst
- A small lump/cyst close to the nail
- Joint deformity
- Joint pain and stiffness
- Skin breakdown or infection
- Nail deformity
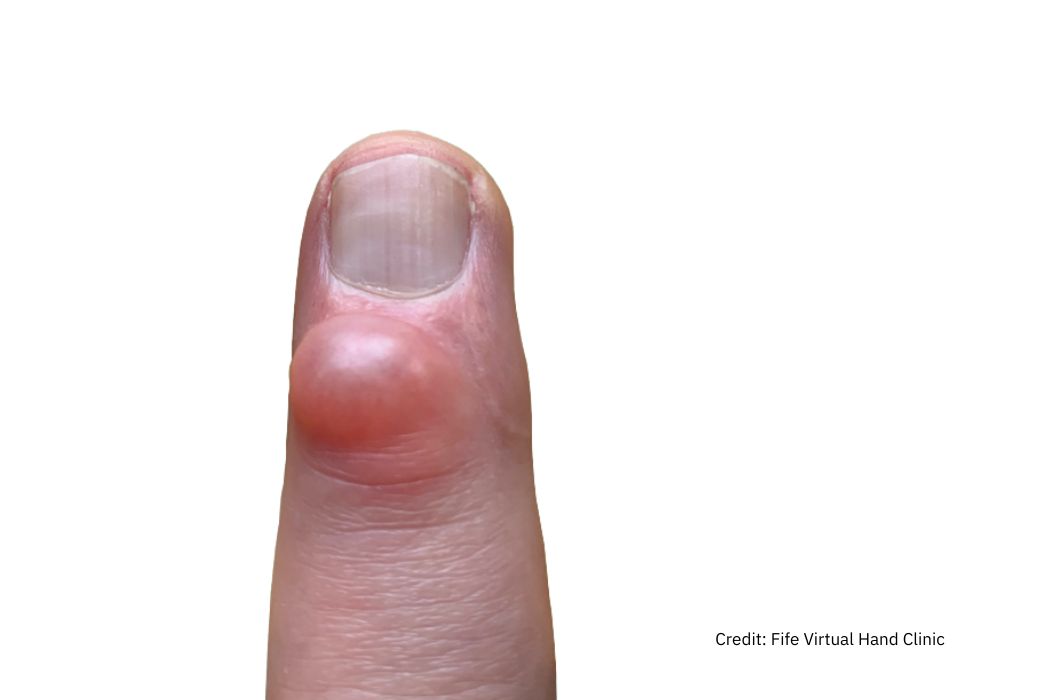
It is a small fluid filled ganglion look alike cyst, that occurs at the end finger joint (DIP joint), on the back of the hand close to the base of the nail.
They are formed by; Small bone hooks around the joint (osteophytes are formed as a result of arthritis of the joint) and Extra fluid from the joint make these small cysts (a reaction of the joint to arthritis).
A digital mucus cyst has clinical features shown in the photograph on the right with the corresponding arthritis at the affected joint on x-ray.
An x-ray will usually show loss of cartilage and osteoarthritis in the joint.

If the digital mucus cyst is not causing any symptoms, it can be left alone. A silicon finger cap can be used to protect the cyst if necessary.
If the digital mucous cyst is causing problems, and the arthritis is mild excision of the cyst and removal of bony extensions of the joint is recommended. The surgery is a day case procedure usually under Local anaesthetic. A finger tourniquet is used to reduce the blood flow to the operation site. The mucus cyst, bony spikes and the affected skin is removed. Sometimes a local skin flap is required to cover the incision if the skin over the joint is very thin. Local anaesthetic is injected for post operative pain relief and a bulky dressing is applied to protect the wound.
If the joint is very arthritic, painful with restricted movements, joint fusion is the best option as otherwise the risk of mucus cyst recurrence will be high. In these situations, the joint is excised through the same incision. A screw is inserted across the joint from the tip of the finger to fuse the 2 bones of the finger together. This will stop the movement at the joint in exchange for long term pain relief.
Hand should be kept dry and clean until the stitches are removed. One week after the procedure the dressing are reduced by the practice nurse and the sutures are removed in the clinic 2 weeks after surgery.
Hand therapy will be arranged to allow gentle range of motion activities.
When joint fusion procedure is carried out, the joint is immobilised in a splint (made by the hand therapist) for 6-8 weeks.

As there is often one digit is involved, there is no driving restriction. However you can not drive on the day of your surgery.
Your return to work will depend on your job. Light manual workers can return to duty in 2 – 3 weeks. Heavy manual workers can return to work after 6-8 weeks.

Please use this form if you are interested in booking an appointment. We do not give general medical advice over email.