Mallet finger develops as a result of injury to the tendon (extensor tendon) that inserts to the tip of the finger and straightens the finger. A direct blow or sudden pressure to the tip of the finger that forcefully bends the finger can either rupture the tendon or pull a little piece of bone from the distal phalange along with the tendon. On this page we will discuss the symptoms and treatments of Mallet Finger.

Mallet Finger Treatment
Book AppointmentSymptoms of Mallet Finger
- Pain and swelling
- Inability to straighten the finger actively
Investigations
An X-ray is usually required to confirm if there is also a bony fragment pulled with the tendon.
Diagnosis
Clinical examination usually confirms the diagnosis. The affected finger does not straighten, no matter how hard the patient tries.

Mallet Finger Treatments Available
The majority of mallet finger injuries can be treated conservatively. If the x-ray shows the tendon has just pulled away without a bony fragment, a non operative treatment in a splint will lead to satisfactory results in most patients. A splint is applied to the back (A) or front (B) of the finger to straighten the joint. It is worn for 6 weeks constantly (day and night) followed by 6 weeks only at night time.
The splint can be removed for washing however I do not recommend this. When the splint is removed during the first 6 weeks, the tip of the finger should be kept straight so that the healing part of the tendon does not break again. As this is quite difficult to achieve, I recommend keeping the splint on constantly for 6 weeks.
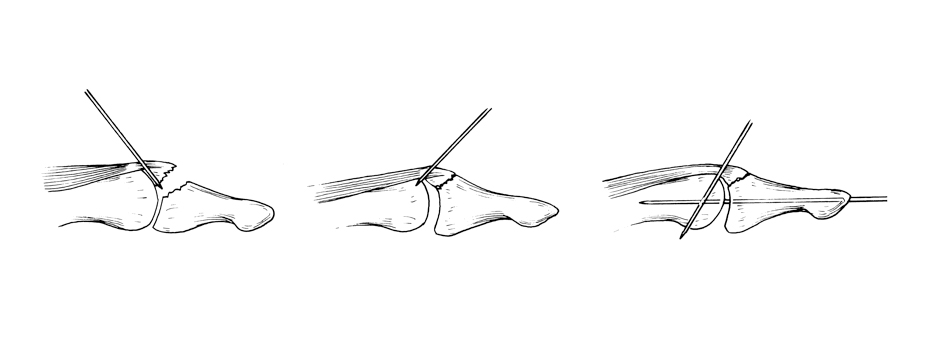
If an x-ray reveals the tendon has pulled off a large fragment of bone with it and there is a significant displacement, surgery may be required.
The surgery is a day case procedure and under local anaesthetic. Small wires are used to approximate and hold the fragments together. The wires are removed at 6 weeks in the clinic. A splint may be required to protect the joint at night time.
Aftercare & Follow Up
Hand should be kept dry and clean until the wires are removed. One week after the procedure the dressing are reduced in the clinic and a splint is made by the hand therapist to protect the finger and the wires. At 6 weeks following the surgery, the wires are removed and the joint movements are guided by the hand therapist.
Driving
Driving may not be restricted if the patient is able to control or maneuver the car confidently.
Time off work
Your return to work will depend on your job. Light manual workers can return to duty in 2 – 3 weeks. Heavy manual workers should not exert maximal grip for 8-10 weeks.
Risk of surgery
- Infection
- Skin breakdown (from splint pressure)
- Injury to the joint and tendon
- Recurrence
- Further surgery (in event of recurrence or other complications)
- Reduced grip strength
- CRPS (chronic pain syndrome: A small percentage of patients will develop a severe reaction after hand surgery, with lifelong permanent pain and stiffness which requires extensive physiotherapy and pain medication).
Book an appointment
Please use this form if you are interested in booking an appointment. We do not give general medical advice over email.